bimonthly assessment january
Headache since 8 days
Fever
since 4 days
Vomitings since 4 days
Altered sensorium since 1 day
1. Hyponatremia secondary to SIADH
2. Tubercular meningitis
3. Acute infarct in the left thalamic region
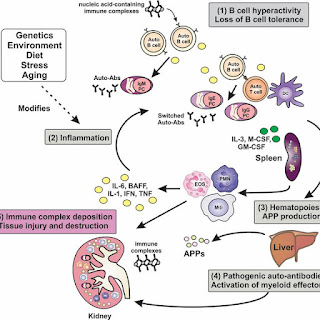
4. SLE with multiple joint pains
Patients with TBM had significantly longer SLE duration, higher ESR and CRP level, and lower CD4+ cell counts and albumin level than those without infections (p < 0.05 for all). There were no differences in prednisone dose at the time of symptom onset or cumulative dose over the preceding year between the two groups. Logistic regression analysis showed that patients with a lower CD4+ cell count were more likely to have TBM compared with controls (OR = 3.67, p = 0.020).
TBM should be considered when SLE patients have central nervous system (CNS) symptoms with a longer duration, higher ESR and CRP level, and lower CD4+ cell counts and albumin level, even if the patients are receiving a low prednisone dose,and the patient being studied has a chronic headache and fits into this criteria
https://pubmed.ncbi.nlm.nih.gov/17338735
P - 441 patients with ischaemic stroke but not complete paresis were included. No antiplatelet drugs were allowed within the last 72hrs before onset. Delay until first trial dosage was maximized to 48hrs.
I - 220 patients received Aspirin (325mg)
C - 221 patients received placebo

4. Please mention your individual learning experiences from this month.
Family history, Smoking, Hypertension, increased BMI, increased Abdominal girth, Dyslipidemia and Diabetes Mellitus and male sex are the main risk factors
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3809218/
https://pubmed.ncbi.nlm.nih.gov/22825899/
b.The initial ecgs shows irregular rhythm along with VPS
There are progressive ST segment changes in the anteroseptal leads - ? STEMI involving LAD territory/ LAD aneurysm
c.https://www.sciencedirect.com/science/article/pii/S0735109702018703
P.
A randomized trial of transfer for primary angioplasty versus on-site thrombolysis in patients with high-risk myocardial infarction: The air primary angioplasty in myocardial infarction study
The Air Primary Angioplasty in Myocardial Infarction (PAMI) study was designed to determine the best reperfusion strategy for patients with high-risk acute myocardial infarction (AMI) at hospitals without percutaneous transluminal coronary angioplasty (PTCA) capability.
I.
Patient selection
Patients were considered if they had either ST-segment elevation or presumed new left bundle branch block and the onset of AMI was <12 h. In addition, one or more of the following criteria for high risk had to be met: age >70 years, heart rate >100 beats/min, systolic blood pressure (BP) <100 mm Hg in the absence of volume depletion, Killip class II/III or an electrocardiogram (ECG) demonstrating left bundle branch block or anterior MI.
Patients were excluded from study participation if they were ineligible for thrombolytic therapy (history of stroke or transient cerebral event in the last six months, major surgery or active gastrointestinal bleeding within the previous two months, organ biopsy within two weeks, cardiopulmonary resuscitation lasting ≥10 min or resulting in rib fracture, systolic BP >200 mm Hg or diastolic BP >110 mm Hg), had cardiogenic shock (defined as systolic BP ≤80 mm Hg in the absence of bradycardia or requiring vasopressors) or had a life-expectancy of less than one year. The study was conducted according to the principles of the Declaration of Helsinki, and all patients gave written, informed consent.
Eligible high-risk patients were randomized to receive either emergent transfer for primary PTCA or on-site thrombolytic therapy. Randomization was stratified by site and accomplished by either telephone randomization from the study coordinating center (U.S. sites) or sealed envelope (non-U.S. sites). The protocol recommended low-flow nasal oxygen, nitroglycerin, oral aspirin (325 mg) and intravenous beta-blockers. Anti-arrhythmic agents and calcium blockers were not routinely administered. Heparin was given according to the treatment arm to which the patient was assigned.
Transfer for primary PTCA arm
For patients randomized to primary angioplasty, emergency transfer was arranged by the most expedient means (either air or ground transport) to the assigned interventional facility. As soon as possible after randomization, a bolus of intravenous heparin was administered, but a continuous infusion was not recommended.
Patients were taken to the cardiac catheterization laboratory immediately upon arrival. Coronary angiography and left ventriculography were performed using low-osmolar ionic contrast medium (ioxaglate, Mallinckrodt, Inc., St. Louis, Missouri). A coronary intervention was performed unless the following exclusions precluded PTCA: infarct vessel stenosis ≤70%, an infarct vessel supplying so little to the myocardium that the PTCA risk outweighed the benefit, unprotected left main stenosis >60% or disease requiring coronary artery bypass graft surgery (CABG). The goal of angioplasty was restoration of normal coronary flow with minimal residual stenosis. Stenting was encouraged for residual lesions >30% or the presence of a coronary dissection. The activated clotting time was maintained at >350 s, and administration of thrombolytic agents was discouraged.
Thrombolytic treatment arm
Patients randomized to thrombolytic therapy received the drug that was considered the standard of care for the participating hospital. If tissue plasminogen activator was administered, heparin was given as an intravenous bolus, followed by an infusion for 72 h, with the dose adjusted to raise the activated partial thromboplastin time between 60 and 80 s. If streptokinase was given, heparin was administered according to the usual practice of the patient’s physician. Patients randomized to thrombolysis remained at the enrolling hospital unless it was the usual practice to transfer patients with AMI. For patients with persistent chest pain, recurrent chest pain or hemodynamic instability, it was recommended that emergency catheterization be considered.
C.Patients with high-risk AMI at hospitals without a catheterization laboratory may have an improved outcome when transferred for primary PTCA versus on-site thrombolysis; however, this will require further study. The marked delay in the transfer process suggests a role for triaging patients directly to specialized heart-attack centers.
Clinical outcomes
Patients randomized to transfer for primary PTCA had a shorter length of hospital stay (6.1 ± 4.3 vs. 7.5 ± 4.3 days, p = 0.015) and less ischemia (12.7% vs. 31.8%, p = 0.007) (Fig. 1). At 30 days, 8.4% of patients randomized to transfer reached the primary end point of death, non-fatal reinfarction or disabling stroke, compared with 13.6% of patients in the on-site thrombolysis group (odds ratio [OR] 0.571, 95% confidence interval [CI] 0.191 to 1.709, p = 0.331). In a secondary, pre-specified analysis using step-down, multivariate, logistic regression, randomization to transfer for primary PTCA was independently associated with a reduction in the primary end point (OR 0.159, 95% CI 0.031 to 0.820, p = 0.028) (Table 4).
Mechanism of benefit of primary PTCA
Transfer to a hospital where the patient will be managed by a cardiologist may result in greater utilization of proven medical therapies (17). We did not find this, but participating centers may not be representative of a non-study situation. Paradoxically, we found greater utilization of beta-blockers in the thrombolytic group, possibly due to treatment of recurrent angina, which occurred more frequently after thrombolytic therapy. Avoiding the use of thrombolytic agents clearly reduces the risk of intracranial bleeding (4), and previous randomized trials have shown reduced rates of reinfarction with PTCA 1, 2, 3, 4. Primary angioplasty reduces the coronary stenosis that may predispose the vessel to reocclusion 18, 19, 20, and it avoids the platelet-aggregating effects of thrombolytic agents 21, 22. Trials with angiographic follow-up suggest that patients treated with primary PTCA 2, 23, 24have substantially lower rates of reocclusion, compared with those treated by thrombolytic therapy 18, 19, 25, 26, and reocclusion may be further reduced by stent placement (27). The greatest benefit of primary PTCA may be its ability to achieve >90% rates of normal coronary flow (28)even when the patient is treated in the late stages of infarction 13, 14. By contrast, thrombolytic therapy has a marked decrease in thrombolytic efficacy in patients treated more than a few hours after symptom onset 9, 10.