1) A 55 year old man with Recurrent Focal Seizures
1. A 55 yr old man who is diabetic alcoholic and chronic smoker came with complaints of weakness of right upper limb right upper limb monoparesis and GTCS may be due to infarct in temporoparietal region
2.as cortical fibres are supplied directly by larger artery (main or only supply) and sub cortical are supplied by smaller branches it is simple to occluded smaller ones( end arteries ) thus sub cortical infarcts are more common
3.ischemia hemorrhage will lead to increased permeability and increased neuronal excitability and seizure threshold is decreased will lead to seizures
4 it is ventricular fibrillation with left axis deviation enoxaparin should be given
https://www.sciencedirect.com/science/article/pii/S0735109702029017
5.
- As it is focal seizure i would prefer carbamazepine
- And lorazepam / diazepam to prevent the conversion of focal seizure to GTCS
Antiepileptics https://pubmed.ncbi.nlm.nih.gov/28661008/
Atorvastatin https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6036014/
Aspirin https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6206448/
Enoxaparin https://www.sciencedirect.com/science/article/pii/S0735109702029017
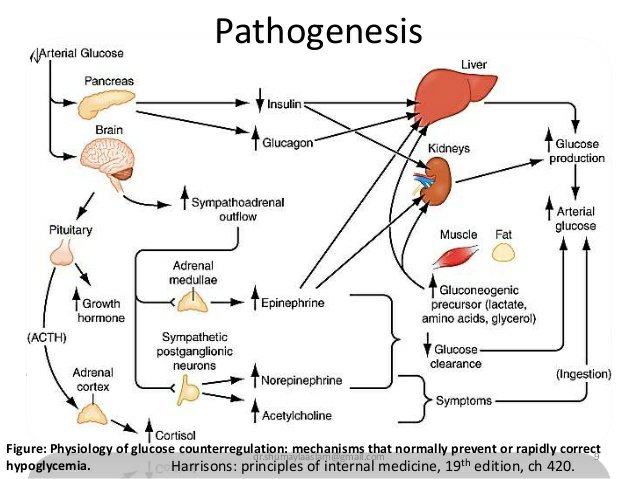
Question 2) 55 year old man with Recurrent hypoglycemia
1.A 55 y old male who is hypertensive and diabetic presented with sob and cough since 3 days and as grbs is decreased it could be overdose of hypoglycemic agent
2.improper usage of anti diabetic drugs without taking proper diet and even only excessive alcohol can increase the hypoglycemia as alcohol increases the insulin production and if he does not take the drink the other day will result in hypoglycemia
Glimipiride will increase insulin secretion that can lead to hypoglycemia compared to other type of drugs
Insulinoma can lead to hypoglycemia
3.as there is prolonged hypoglycemic state it will lead break down of lipids and proteins that way it will decrease albumin in the body and increased anaerobic pathways will lead to accumulation lactic acid and respiratory acidosis will lead to dyspnea
4.
5.Usage of antibiotics is questionable
But as he is diabetic he is prone to any type of infection
3.A.41 year old man with Polyarthralgia
1.41 yr old male with early morning stiffness of smaller joints along with larger joints so it is rheumatoid arthritis which explained by fever and joint pains and pericarditis due to the murmur
ra factor negative can further be evaluated by anca and anti ccp and diagnosis is mainly by eular criteria
2.In the initial disease stage there are qualitative and quantitative disturbances ofpeptide citrulination as well as other protein modifications, followed by antigen presenting cell (APC) (macrophages and dendritic cells) and fibroblast like synoviocytes (FLS) activation. Some microbes foster this processes by APC and FLS direct and indirect activation. In the second stage APC's elicit specific humoral B cell re- sponse resulting in specific antibodies production and T cell autoreactivity. Inherited and acquired defects in T and B cell responses caused by repeated activation of innate immunity as well as loss of tolerance, elicit chronic autoimmune inflammation, primarily of synovial membranes, and development of cellular panus. Pathologic activation of the osteoclasts and release of the immune system effector molecules and the proteolytic enzymes damage the cartilage, bone and tendons composition and structure. Persistent inflammation through its complex mechanisms results in many systemic and extraarticular RA manifestations of almost all organ systems, resulting in severe complications and comorbidities such as rheumatoid lung, carditis, vasculitis, cahexia, anemia, accelerated atherosclerosis, myocardial and cerebrovascular vascular disease, lymphoma, osteoporosis, depression etc. Accumulated complications and comorbidities finally result in handicap, social dysfunction and premature death.
3 b 75 year old woman with post operative hepatitis following blood transfusion
1.Post transfusion delayed hemolytic reaction
Evaluation:
- ABO and Rh compatability
- coombs testing
- antibody panel testing
https://www.learnhaem.com/courses/frcpath-transfusion/lessons/antibody-screening-and-identification/topic/antigrams/
Transfusion related acute hepatic injury (TRAHI)
- -Post transfusion hepatitis
- -Ischemic hepatitis
Evaluation:
2. What would be your treatment approach? Do you agree with the treatment provided by the treating team and why? What are their efficacies?
Symptomatic management
I agree with the treatment provided by the treating team
Lasix & Nebulization : For wheezing and crepts
Lactulose : To prevent hepatic encephalopathy https://pubmed.ncbi.nlm.nih.gov/27089005/
Zofer : For vomitings
Pantop : To prevent gastritis
4)60 year old woman with Uncontrolled sugars
1.chest pain -radiating to epigastrium and back
uncontrolled sugars
leucocytosis secondary to ?community acquired pneumonia
?lung abscess
no further history mentioned in terms of fever , cough, sob
2)reason for uncontrolled sugars
sepsis
poor glycemic control prior to hospital administration with hba1c 8, (history not clear about compliance)
https://www.semanticscholar.org/paper/Stress-hyperglycemia%2C-insulin-and-immunomodulation-Marik-Raghavan/24f1499f7360fc0564d7f66cee5cfa7953c73616
Changes in whole-body glucose uptake and glucose oxidation in sepsis are complex and may depend on the severity of illness and the stage of the disease. Wholebody glucose uptake and glucose oxidation may be increased in the early stages of sepsis and endotoxemia [25, 26]. This may be the result of cytokine-induced increase in non-insulin mediated glucose uptake by tissues rich in mononuclear phagocytes, including the liver, spleen, ileum, and lung [27, 28]. Enhanced noninsulin mediated glucose uptake appears to result from an increase in the synthesis, concentration or activity of the GLUT1 transporter [29, 30]. With the development of insulin resistance glucose utilization and oxidation may decrease [25, 31, 32]. Exogenous insulin increases glucose utilization and oxidation; however, nonoxidative disposal (storage) remains impaired [25, 31
3.the xray findings in this pt are
p/a view ,adequate exposure with opacities in right upper lobe ,
with air bronchogram, with bulging fissure sign suggestive of lobar consolidation
4) hypoalbunemia
https://www.dvm360.com/view/approach-hypoalbuminemia-proceedings
The potential causes of hypoalbuminemia are many, and include:
Hepatic failure (failure of albumin synthesis)
Gastrointestinal protein loss (protein-losing enteropathy)
Renal protein loss (protein-losing nephropathies)
Other external losses in exudate or hemorrhage
Hyperglobulinemia (with a 'compensatory' decrease in albumin production)
Starvation/protein malnutrition
Chronic illness
Hypoadrenocorticism
Laboratory error
the cause in this patient can be attributes to malnutrition or albumin as acute phase reactant
https://onlinelibrary.wiley.com/doi/10.1002/jpen.1451
Inflammation increases capillary permeability and escape of serum albumin, leading to expansion of interstitial space and increasing the distribution volume of albumin. The half‐life of albumin has been shown to shorten, decreasing total albumin mass. These 2 factors lead to hypoalbuminemia despite increased fractional synthesis rates in plasma.
5.
treatment efficacies
piperacillin tazobactum
https://pubmed.ncbi.nlm.nih.gov/9721959/
A favorable clinical response was observed in 90% of the piperacillin/ tazobactam group and in 84% of the co-amoxiclav/aminoglycoside group (not significant). The bacteriological efficacy was comparable in both groups
clarithromycin
https://journal.chestnet.org/article/S0012-3692(15)42279-2/abstract
5) 56 year old man with Decompensated liver disease
1.
- Liver : Chronic liver disease (cirrhosis) secondary to HBV
- Kidney : AKI on CKD (Hepatorenal syndrome) , Hyperkalemia
- GI : GAVE , portal hypertensive gastropathy
- Lung : pneumonia , pleural effusion
2.
The initial evaluation of the patient found to have hepatitis B surface antigen (HBsAg) in serum should attempt to establish the diagnosis and assess the grade of the disease.
These phases include
1. An early, immune-tolerant phase that typically occurs in children and is marked by high levels of HBV DNA, presence of HBeAg, but normal serum aminotransferase levels and absence of disease activity
2. Immune activation phase of chronic hepatitis B, marked by moderate to high levels of HBV replication, continued or fluctuating disease activity and aminotransferase elevations and during which progressive liver damage can occur and
3. An inactive carrier state, marked by low levels of HBV replication, absence of HBeAg and normal serum aminotransferase levels with inactive liver disease.
Chronic hepatitis B is a dynamic disease, and patients can pass from one phase to another and back, from disease activity to inactivity. During periods of activity, progressive liver damage can occur, resulting in cirrhosis and its complications, as well as hepatocellular carcinoma (HCC).
Thus, the presence of HBsAg in serum may have a range of implications, indicating acute or chronic hepatitis B that can be mild or severe and progressive. The goals of the initial evaluation should be to determine the phase of HBV infection, the severity of disease, and the need for monitoring and treatment.
3.
HBV attaches to the host hepatocyte cell membrane through its envelope proteins. When the viral membrane fuses with the cell membrane, it will result in releasing the viral genome into the cell cytoplasm. After the viral genome reaches the nucleus, the viral polymerase enzyme will convert the partially double-stranded DNA genome into cccDNA. This is followed by transcription and nuclear export of all viral mRNA to the cytoplasm for translation. The surface protein enveloping process occurs in the endoplasmic reticulum and then assembled in the cytoplasm. These proteins are transported to the post-endoplasmic reticulum and Golgi compartments for the budding of the nucleocapsid. The different viral components will assemble into new virions that will be released out of the host and infect new hepatocyte.
- Yes , separate machines must be used for patients known to be infected with HBV (or at high risk of new HBV infection). A machine that has been used for patients infected with HBV can be used again for non-infected patients only after it has been decontaminated using a regime deemed effective against HBV because of increased risk of transmission due to contamination.
https://bmcnephrol.biomedcentral.com/articles/10.1186/s12882-019-1529-1
5. Lactulose : for prevention and treatment of hepatic encephalopathy. https://pubmed.ncbi.nlm.nih.gov/27089005/
Tenofovir : for HBV
Octreotide : for upper GI bleed. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1750992/#:~:text=In%20a%20meta-analysis%2C%20somatostatin,(mostly%20caused%20by%20gastritis).
Lasix : for fluid overload (AKI on CKD) 0https://www.ncbi.nlm.nih.gov/books/NBK499921/#:~:text=The%20Food%20and%20Drug%20Administration,failure%20including%20the%20nephrotic%20syndrome.
Vitamin -k : for ? Deranged coagulation profile (PT , INR & APTT reports not available)
Pantop : for gastritis
Zofer : to prevent vomitings
Monocef (ceftriaxone) : for AKI (? renal)
6.) 58 year old man with Dementia
1. What is the problem representation of this patient?
A 58 year old weaver occasional alcoholic c/o slurring of speech , deviation of mouth to right side associated with drooling of saliva , food particles and water predominantly from left angle of mouth and smacking of lips since 6 months.Urinary urge incontinence since 6 months.
Forgetfulness since 3 months.
He has delayed response to commands.
Dysphagia to both solids and liquids since 10 days.
K/c/o CVA 3 years back and now he was diagnosed as neuro degenerative disease - Alzheimer's (? Vascular - post stroke sequale)
2. How would you evaluate further this patient with Dementia?
Yes dementia can be coexplained by infarcts
4.
5.
PHARMACOLOGIC:
Cholinesterase inhibitors:
- Donepezil
- Rivastigmine
- Galantamine
NMDA antagonist:
- Counselling the patient and care givers
- Geriatric care
- Cognitive / emotion oriented interventions
- Sensory stimulation interventions
- Behaviour management techniques
Efficacy:
7) 22 year old man with seizures
1.
A 22 year old delivery boy chronic alcoholic and tobacco chewer c/o on & off fever since 1 year , involuntary weight loss since 6 months , headache since 2 months , 4 - 5 episodes of involuntary stiffening of both UL & LL with 5 min LOC 1 week before the day of admission.
Brain - multiple ring enhancing lesions in right cerebellum ? Tuberculoma
RVD positive
2.
Bacterial
Pyogenic abscess
Tuberculoma and tuberculous abscess Mycobacterium avium-intracellulare infection Syphilis
Listeriosis
Fungal
Nocardiosis
Actinoimycosis
Rhodococcosis
Zygomycosis
Histoplasmosis
Coccidioidomycosis
Aspergillosis
Mucormycosis
Paracoccidioidomycosis
Cryptococcosis
Parasitic
Neurocysticercosis
Toxoplasmosis
Amoebic brain abscess
Echinococcosis
Cerebral sparganosis
Chagas' disease
Neoplastic
Metastases
Primary brain tumor
Primary CNS lymphoma
Inflammatory and demyelinating
Multiple sclerosis
Acute disseminated encephalomyelitis
Sarcoidosis
Neuro-Behcet.s disease
Whipple's disease
Systemic lupus erythematosus
3.
A paradoxical clinical worsening of a known condition or the appearance of a new condition after initiating anti retroviral therapy (ART) therapy in HIV-infected patients resulting from restored immunity to specific infectious or non-infectious antigens is defined as immune reconstitution inflammatory syndrome (IRIS).
As his CD4 count is > 50 /mm3 consider delayed initiation of ART ideally after 8 weeks of starting ATT to reduce the chances of developing IRIS
8. Cardiorenal syndrome
Points about cardiac murmurs
Vats
Status epilepticus
Cortical infarcts evaluation
HIV pts with iris